CRISPR gene editing has emerged as a revolutionary force in modern science, allowing researchers to manipulate genetic material with unprecedented precision. Through CRISPR technology, scientists can target and alter specific genes, presenting new possibilities for treating genetic disorders like sickle cell anemia. However, the rapid advancement of gene editing raises critical ethical implications that society must grapple with. As we delve deeper into the potential and risks associated with this innovative approach, questions around health equity in gene therapy and the moral responsibilities of altering human DNA come to the forefront. Ultimately, the journey into gene editing is not just a scientific exploration but a profound ethical debate that challenges our understanding of what it means to be human.
Gene editing, particularly through advanced techniques like CRISPR, offers groundbreaking potential for altering our genetic makeup, thereby opening up discussions about our right to modify human attributes. This innovative approach to genetic manipulation can target and repair mutations, proposing solutions for conditions such as sickle cell disease. Yet, while the benefits are promising, the conversation inevitably leads to concerns surrounding the ethical ramifications of these alterations. As advancements in genetic modification continue to evolve, the focus on responsible practices and equitable access to such treatments is crucial. Engaging with these considerations ensures that as we push the boundaries of science, we also uphold the values of justice and human dignity.
Understanding CRISPR Technology and Its Applications
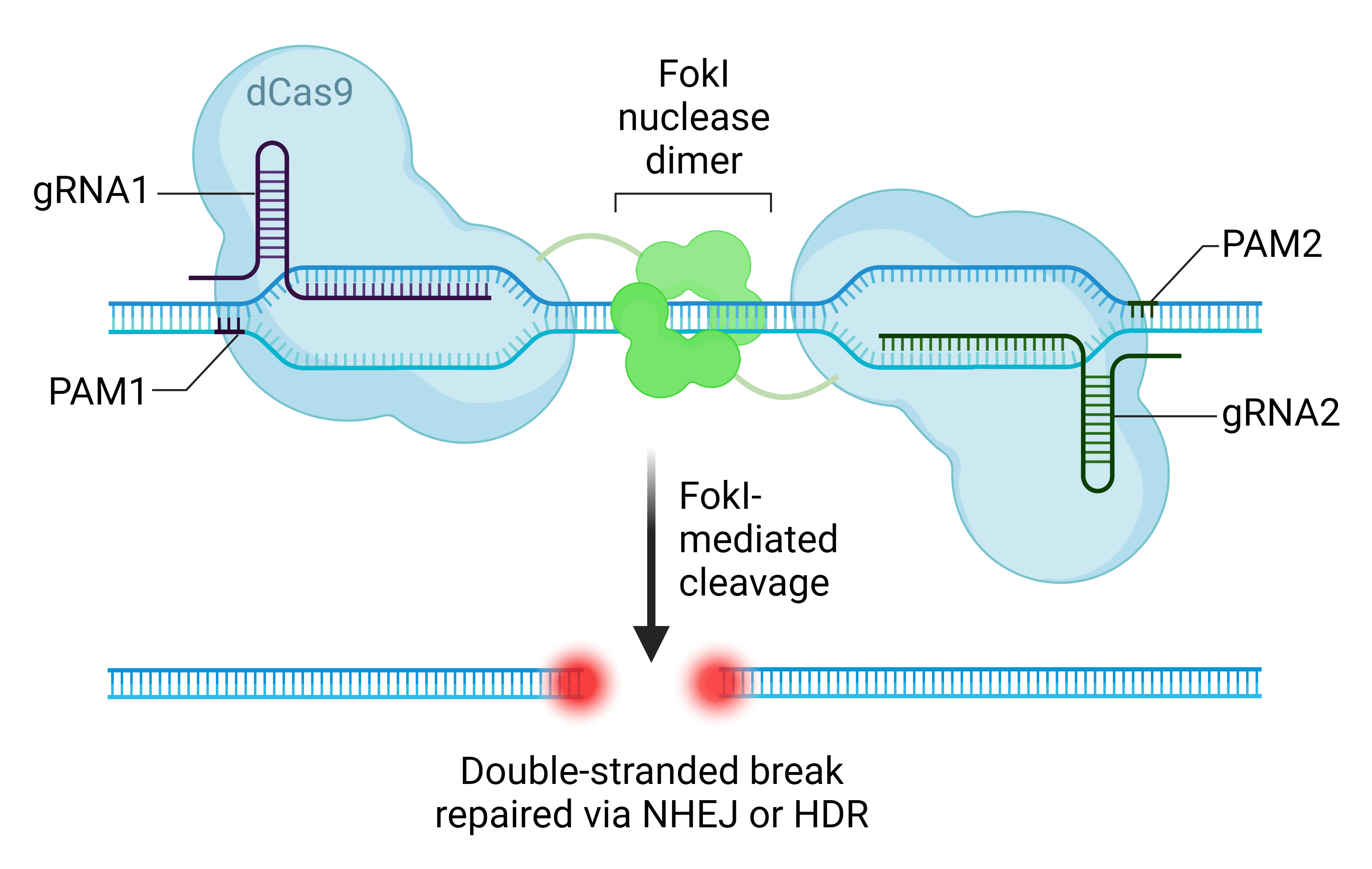
CRISPR gene editing has emerged as a groundbreaking tool in the realm of genetics, revolutionizing the way we approach genetic diseases. This technology allows precise modifications of DNA, targeting specific genes responsible for conditions such as sickle cell anemia. By utilizing the CRISPR-Cas9 system, scientists can effectively snip out defective genetic sequences and introduce healthy ones, thereby holding the potential for cures that seemed impossible just a few decades ago. The ability to edit both somatic and germline cells creates new possibilities for not only treating diseases but also potentially preventing them from being passed down through generations.
Despite the excitement surrounding CRISPR technology, its applications come with a host of ethical quandaries. One of the most pressing debates centers on whether it is appropriate to use gene editing for conditions that do not severely impact quality of life. For instance, should parents be allowed to modify genetic traits that may lead to certain syndromes when those affected individuals can lead fulfilling lives? This dilemma emphasizes the need not just for scientific advancement, but also for a robust dialogue on the moral implications of playing ‘God’ with human genes.
Ethical Implications of Gene Editing
The ethical implications of gene editing are significant and varied, touching on issues of consent, equity, and the very definition of what it means to be human. As discussed in Neal Baer’s talk at Harvard, these technological advancements in CRISPR gene editing challenge our understanding of health and wellness. The risk of exacerbating inequality in healthcare access is a primary concern; as advancements in gene editing often come at a high financial cost, they could widen the gap between wealthy individuals who can afford treatment and those who cannot. This scenario raises troubling questions about health equity and justice in medicine.
Moreover, there is the issue of oversight and regulation in gene editing practices. The absence of a unified global stance on genetic modification can lead to ethically questionable practices in countries where such advancements are poorly monitored. Baer pointed out the dangers of unchecked gene editing, particularly in cases where military applications may arise, such as genetically modifying soldiers for enhanced physical endurance or resilience. As the conversation continues, it becomes evident that ethical guidelines must evolve alongside technology to safeguard against potential exploitation and abuse.
The Promise of Sickle Cell Anemia Gene Therapy
Sickle cell anemia is one of the most significant hereditary disorders affecting thousands of individuals globally, and CRISPR gene editing provides a promising avenue for therapeutic intervention. With the capacity to directly edit the genes responsible for this painful condition, researchers have demonstrated that CRISPR can effectively eliminate the faulty genes from patients’ bone marrow cells, potentially leading to a complete cure. This level of precision could transform the lives of many children and adults suffering from the debilitating effects of sickle cell disease, presenting a much-needed solution to a longstanding medical challenge.
However, as promising as CRISPR technology may be for sickle cell gene therapy, its implementation is not without challenges. The high costs associated with these treatments, often ranging in the millions, raise ethical concerns surrounding who will have access to such transformative therapies. The disparity in healthcare resources highlights the need for a greater focus on health equity to ensure that life-saving technologies like CRISPR are available to all patients, regardless of their socio-economic status. The hope is that as research continues, the benefits of gene editing can be made accessible to a broader population.
Gene Editing Risks: A Cautionary Tale
While CRISPR technology offers immense potential in treating genetic disorders, it also carries inherent risks that must be diligently considered. Gene editing is not without the possibility of unintended consequences; the alteration of one gene can inadvertently affect others, resulting in unforeseen health issues. For example, while researchers have made significant advancements in reducing LDL cholesterol through gene editing, the complex nature of genetic interactions means that altering one gene may inadvertently disrupt others critical to metabolic functions.
Beyond biological risks, the societal implications of gene editing also pose serious concerns. The potential for ‘designer babies’ and selective genetic traits creates ethical dilemmas regarding who decides which genes are desirable. The variability in gene editing outcomes can lead to a broader conversation on societal norms and expectations, potentially leading to a new form of discrimination based on genetic traits. It is essential for scientists, ethicists, and policy makers to engage in an ongoing dialogue about these risks to ensure responsible and equitable use of gene editing technology.
Health Equity in Gene Therapy: Bridging the Gap
In discussions surrounding CRISPR gene editing, health equity has emerged as a pivotal theme. The disparity in access to gene therapies, such as those being explored for sickle cell anemia and other genetic conditions, underscores the need for a unified ethical framework that prioritizes fairness in healthcare. As new technologies are introduced, it is crucial that they are accessible not only to the affluent but also to marginalized communities who have historically been underserved by the healthcare system.
Promoting health equity in gene therapy requires collective efforts from all stakeholders involved, including researchers, healthcare providers, and policymakers. It is essential to create policies that prioritize funding for treatments that are scientifically sound, yet also equitable. Through community engagement and understanding the social determinants of health, solutions can be crafted that ensure everyone, regardless of their socio-economic background, can benefit from advancements in gene editing and gene therapy.
The Role of Bioethics in Gene Editing Discussions
The field of bioethics plays a critical role in navigating the complex landscape of CRISPR gene editing. As breakthroughs in genetic engineering continue to emerge, it is vital to incorporate ethical considerations into scientific research and its applications. Experts like Rebecca Weintraub Brendel advocate for a collaborative approach that brings together researchers, ethicists, and affected communities to address the multifaceted implications of gene editing technologies. By fostering dialogue and asking tough questions about intent and impact, bioethics can guide responsible use in a rapidly evolving field.
Engaging bioethics ensures that the benefits of CRISPR gene editing are pursued alongside appropriate safeguards against misuse. There is a growing movement advocating for ethical frameworks that prioritize informed consent, respect for personal autonomy, and the potential societal effects of genetic manipulation. As we stand on the precipice of genetic revolution, embedding ethical considerations into the heart of scientific inquiry will not only protect individuals but also help shape a future that promotes justice and equity in health.
Public Perception and Gene Editing
Public perception of CRISPR gene editing greatly influences its acceptance and application within society. As advancements in genetic technology become more widely discussed, so do the various opinions regarding the moral implications of editing the human genome. A significant contingent of the public expresses concern over the unforeseen consequences that gene editing could bring, especially when considering its potential to alter human life in profound and irreversible ways. These concerns underscore the necessity for transparent communication and public education about the risks and benefits of gene editing.
Moreover, understanding how the public views CRISPR technology is crucial for policymakers and researchers alike. Engaging with communities to address their apprehensions, misconceptions, and hopes regarding gene editing fosters a more inclusive approach to scientific progress. By cultivating informed public discourse, stakeholders can help shape policies that reflect community values and ethical boundaries while still embracing the tremendous potential of CRISPR technology in addressing genetic diseases.
Navigating the Regulatory Landscape of Gene Editing
As gene editing technologies like CRISPR become more prevalent, a robust regulatory framework is essential in ensuring their ethical use. Currently, regulations governing genetic modifications vary widely across countries, leading to inconsistencies in practices and ethical standards. These discrepancies can pose significant challenges in terms of safety, oversight, and the global impacts of gene editing technologies. The establishment of international guidelines and agreements may be necessary to create uniform practices that prioritize both innovation and ethical standards.
Additionally, engaging with a diverse group of stakeholders in the regulatory process, including ethicists, scientists, healthcare professionals, and patient advocacy groups, can create a more comprehensive framework. This collaborative approach can ensure that regulations are not just effective but also flexible enough to adapt to the rapid advancements occurring in gene editing. By navigating the regulatory landscape thoughtfully, we can better harness the capabilities of CRISPR technology while addressing the ethical, social, and health equity challenges it presents.
The Future of CRISPR: Opportunities and Challenges
The future of CRISPR gene editing technology holds immense potential for transformative health solutions across various fields. From eliminating genetic disorders like sickle cell anemia to enhancing agricultural resilience, the applications are expansive. Continued research and development could lead to cures for previously untreatable conditions, offering hope to millions. However, with this potential comes a set of challenges that must be acknowledged and addressed to harness CRISPR ethically and responsibly.
Among the challenges are the ethical quandaries related to genetic modification, including the risk of exacerbating health disparities and the potential for ‘designer genes.’ The discourse surrounding these issues calls for a careful consideration of the societal implications of gene editing technologies. Activating a dialogue between scientists, ethicists, and the public is crucial to navigate these complexities, ensuring that the follow-through of CRISPR’s promise is measured against a commitment to justice and equity in healthcare.
Frequently Asked Questions
What is CRISPR gene editing and how does it work?
CRISPR gene editing is a revolutionary technology that allows scientists to alter an organism’s DNA. It works by using a guide RNA to identify specific sequences in the genome, and the CRISPR-associated protein (Cas9) to cut the DNA at those targeted locations. This enables the addition or removal of genetic material to correct genetic defects or modify traits.
What are the ethical implications of CRISPR technology?
The ethical implications of CRISPR technology are significant and varied. Concerns include the potential for eugenics, where individuals may edit traits based on personal preferences rather than medical necessity, raising questions about ‘playing God’ and the definition of normalcy. These discussions also involve considerations of health equity, as the affordability of CRISPR gene editing therapies could widen the gap between those who can afford them and those who cannot.
How does CRISPR technology relate to sickle cell anemia gene therapy?
CRISPR technology is being used to develop therapies for sickle cell anemia by editing the genes responsible for the disease. Researchers can edit somatic cells to eliminate the defective gene causing sickle cell disease, potentially leading to a functional cure. This application exemplifies the potential of CRISPR gene editing to address genetic disorders.
What are the risks associated with gene editing using CRISPR?
While CRISPR gene editing has immense potential, it also carries risks, including unintended edits in the genome, referred to as off-target effects, which could lead to new diseases or complications. Additionally, the long-term effects of gene editing are still not fully understood, making it essential to proceed cautiously in both research and clinical applications.
How does CRISPR gene editing impact health equity in gene therapy?
CRISPR gene editing has the potential to improve health equity by providing cures for genetic disorders like sickle cell anemia. However, there are concerns that the high costs of such treatments might limit accessibility, thus exacerbating existing health disparities. Addressing health equity involves ensuring that advancements in CRISPR technology are accessible to diverse populations, especially marginalized groups.
| Key Aspect | Details |
|---|---|
| Introduction to CRISPR | Focus on ethical implications and potential of gene editing. |
| Personal Experience | Dr. Neal Baer shares his experiences treating children with sickle cell anemia. |
| Benefits of CRISPR | CRISPR can potentially cure illnesses like sickle cell disease. |
| Ethical Dilemmas | Questions arise about modifying genes for conditions like Down Syndrome. |
| Economic Concerns | The cost of gene therapies like sickle cell treatment raises issues of accessibility. |
| Health Justice | Innovation must consider implications for those without resources. |
| Parental Control | Debate over parental rights to decide genetic traits for children. |
| Global Oversight | Concerns about lack of regulation in countries like Russia and China. |
| Unintended Consequences | Altering genes can lead to unpredictable health repercussions. |
Summary
CRISPR gene editing presents groundbreaking possibilities in medicine, especially in curing genetic diseases like sickle cell anemia. However, it also raises profound ethical questions regarding our responsibility to modify human genetics. As we advance in this technology, a careful examination of its implications for health equity, parental rights, and global oversight is critical to ensure that we navigate the promise and peril of gene editing responsibly.