Medical research safety is a paramount concern in the landscape of clinical studies, particularly as it ensures the protection and welfare of research participants. As funding cuts threaten to disrupt vital oversight mechanisms like Institutional Review Boards (IRBs), the rights of patients participating in research could be jeopardized. The IRB’s responsibilities include safeguarding patient safety in research, carefully vetting studies to prevent harm, and ensuring compliance with ethical standards. Without sufficient funding, the critical infrastructure necessary for clinical research oversight may falter, impacting studies at multiple sites and diminishing the integrity of research as a whole. This uncertainty raises alarm about the potential risks faced by those who volunteer to be a part of innovative medical inquiries, highlighting the need for continual vigilance and support to uphold the standards of research participant rights.
In the realm of clinical investigations, the importance of ensuring the safety and well-being of individuals involved cannot be overstated. This aspect, often referred to as research participant protection, encompasses a broad range of ethical considerations and regulatory compliance. The oversight provided by bodies such as Institutional Review Boards (IRBs) is crucial for assessing the safety measures in place and preserving the rights of participants. Recent funding challenges have spotlighted the fragility of these safety nets that underpin medical research, raising concerns over how cuts could diminish the necessary clinical research oversight. As we navigate these challenges, it becomes increasingly vital to emphasize the ethical responsibilities associated with human subjects research and the imperative to maintain robust protections for all involved.
Understanding Patient Safety in Medical Research
Patient safety is a cornerstone of medical research, especially for studies involving human participants. This safety is ensured through rigorous protocols established by Institutional Review Boards (IRBs), which assess and monitor research activities throughout their lifecycle. The IRB’s responsibilities include evaluating study designs, consent processes, and measures to mitigate risks, ensuring that researchers prioritize participant welfare at every stage of a study. Moreover, IRBs provide crucial oversight, which helps to maintain public trust and ensures that the rights of research participants are upheld.
Recent funding cuts, particularly those imposed by the federal government, threaten to disrupt this balance of safety and oversight. Reduced resources mean that fewer personnel are available to perform vital checks on ongoing studies, which can compromise the safety protocols intended to protect patients. Without adequate funding, the capacity to monitor compliance and conduct necessary reviews diminishes, posing serious risks not only to individual participants but also to the integrity of the research community as a whole.
The Role of IRBs in Safeguarding Research Participants
As guardians of ethical research practices, Institutional Review Boards (IRBs) play an indispensable role in the infrastructure of clinical studies. Their primary responsibility is to ensure that all research proposals are carefully scrutinized against ethical standards and that participant rights are protected. This includes evaluating the merit of study designs, participant recruitment methods, and the adequacy of informed consent processes. By promoting transparency and accountability, IRBs serve as the ‘checks and balances’ of medical research.
However, the recent halt in research funding can hinder IRBs in fulfilling these obligations effectively. With diminished financial support, IRBs may struggle to conduct comprehensive reviews or engage in community education regarding participants’ rights. This situation not only threatens the protection of individuals involved in research but could also lead to ethical lapses, affecting the very foundation of trust upon which medical research is built. Without sufficient oversight, the potential for harm increases, emphasizing the importance of robust funding for the maintenance of ethical standards in clinical trials.
Impact of Funding Cuts on Clinical Research Oversight
The freeze on research funding has far-reaching implications for clinical research oversight, significantly threatening the infrastructure that supports ethical and safe medical experiments. The absence of more than $2 billion in federal grants, like those lost through the Trump administration’s funding cuts to institutions like Harvard, disrupts the operational capabilities of IRBs that oversee multiple research sites. This disruption has halted ongoing studies, prevented new site enrollments, and interrupted essential data collection processes, which may lead to incomplete or inconclusive research outcomes.
Furthermore, funding cuts can exacerbate existing inequities in research, potentially sidelining marginalized groups that could benefit from new medical advancements. With diminished resources, the responsiveness of IRBs to community needs may also weaken, reducing their effectiveness in educating participants about their rights and safety. As studies lag, public perception of clinical research may shift towards skepticism, endangering future participant recruitment and the overall progress of medical science. Hence, these cuts not only stall current research but undermine the public’s trust in the scientific process.
The Historical Context of Medical Research Ethics
Understanding the historical context of medical research ethics is crucial for appreciating the modern frameworks of safety and oversight that exist today. Historical atrocities, such as the Tuskegee syphilis study and unethical practices during World War II, highlighted the need for stringent ethical standards in research involving human subjects. These events led to the establishment of IRBs, designed to monitor and ensure that research is conducted ethically and that participant welfare is prioritized.
The evolution of these oversight mechanisms is a testament to society’s commitment to protecting individuals involved in research. However, recent funding cuts present a challenge to this evolution. The resources that sustain IRBs and support their training and operational capacities are critical for maintaining ethical vigilance. As funding dwindles, there is a tangible risk of reverting to a time when unchecked research practices could undermine patient safety and informed consent.
Community Engagement and Research Participant Rights
Community engagement is vital in ensuring that research participants are informed and their rights are respected. Effective communication and collaboration with diverse populations not only enrich the research process but also enhance participant trust. IRBs play a key role in this engagement, facilitating dialogues that empower communities and foster mutual understanding. By actively involving communities, researchers can gather insights that inform study design, recruitment strategies, and dissemination of results.
However, funding cuts jeopardize the ability of IRBs to engage meaningfully with communities and educate potential participants about their rights. The diminishing opportunity for outreach and public education can lead to a disenfranchised participant population, who may lack understanding of their rights and the significance of informed consent. Programs that rely on comprehensive community engagement to build trust and understanding may falter under financial constraints, ultimately affecting the integrity of the research process and diminishing the rights of those who participate.
How the SMART IRB System Enhances Research Efficiency
The SMART IRB system represents a significant advancement in the collaborative review of research protocols, aimed at enhancing efficiency in the oversight of multi-site studies. By enabling a single IRB to review protocols for all participating sites, SMART IRB reduces duplication of effort and accelerates the initiation of clinical trials. This streamlined process not only benefits researchers by saving time and resources but also facilitates quicker access to potentially life-saving treatments for patients.
However, the recent stop-work order stemming from funding cuts curtails the capabilities of the SMART IRB system. As new clinical sites are unable to join ongoing studies, researchers face increased delays, potentially leaving patients without timely interventions. The efficiency that the SMART IRB brought to the research landscape is now at risk, threatening to undo the progress made in collaborative research practices and affecting the overall patient experience in clinical settings.
Navigating Ethical Dilemmas in Medical Research
Navigating ethical dilemmas in medical research requires a delicate balance between scientific inquiry and participant protection. IRBs are tasked with addressing complex ethical questions that arise during research design, implementation, and reporting. They ensure that researchers adhere to ethical principles such as respect for persons, beneficence, and justice. By scrutinizing research proposals against these benchmarks, IRBs safeguard participants’ welfare and rights while fostering innovation.
Nevertheless, the impact of funding cuts introduces new challenges in addressing these ethical dilemmas. Financial constraints may limit the ability of IRBs to consult with ethical experts or to provide adequate training for investigators. The intricacies of navigating ethical issues require vigilance and continuous education; without adequate funding, the diligence needed to uphold ethical research standards may falter. Researchers may inadvertently close critical channels of dialogue concerning ethics, thereby jeopardizing the quality of oversight and the safety of research participants.
The Future of Medical Research Funding and Safety
The future of medical research funding is inextricably linked to the safety and rights of research participants. As funding models continuously evolve, it is critical to advocate for sustained financial support for ethical oversight mechanisms, particularly IRBs. Ensuring that these boards have the necessary resources to evaluate and oversee research is essential for maintaining the integrity of medical studies, protecting patient safety, and upholding the rights of individuals involved in research.
As we face increasing challenges in the realm of healthcare and research, it is imperative that all stakeholders in the research community, including institutions, funding bodies, and the public, recognize the importance of investing in safety protocols. The interplay between adequate funding and the empowerment of IRBs can forge a robust and resilient framework to support ethical research practices that genuinely benefit society. By prioritizing patient safety, we not only honor the rights of research participants but also foster a culture of trust and transparency that is essential for the advancement of medical science.
Rebuilding Trust in Clinical Research Post-Funding Cuts
Rebuilding trust in clinical research is paramount, especially in light of recent funding cuts that compromise oversight and participant safety. Trust is foundational to the research enterprise, as it encourages willing participation by individuals from diverse communities. To cultivate this trust, research institutions must commit to transparency in their practices, actively communicate the safeguards that protect participants, and engage communities in meaningful dialogue about their rights and involvement.
Moreover, collaboration between research institutions and the public can lead to enhanced understanding of the research process, ensuring that participants feel valued and recognized. As the research landscape evolves after funding cuts, establishing strong partnerships with communities will be essential to rebuilding trust and demonstrating a shared commitment to ethical practices. Through continuous engagement and advocacy for the rights of participants, we can restore confidence in clinical research and foster a culture that prioritizes safety and respect.
Frequently Asked Questions
How does patient safety in medical research get ensured?
Patient safety in medical research is ensured through rigorous review and oversight by Institutional Review Boards (IRBs). These boards assess research proposals to ensure compliance with ethical standards, safeguard participant rights, and mitigate risks associated with clinical trials.
What are the responsibilities of IRBs in relation to patient safety in research?
IRBs are responsible for reviewing research protocols, monitoring informed consent processes, evaluating risks and benefits, and ensuring that the rights and welfare of research participants are protected throughout the study.
How do funding cuts impact medical research safety?
Funding cuts threaten medical research safety by halting essential safety oversight provided by IRBs. When research funding is reduced, studies may be paused or canceled, which can compromise the welfare of participants and lead to distrust in the research process.
Why are research participant rights critical for patient safety in medical research?
Research participant rights are essential for patient safety as they empower individuals to make informed decisions about their participation. Respecting these rights helps ensure ethical conduct of research and promotes trust between researchers and participants.
How does clinical research oversight contribute to patient safety?
Clinical research oversight, primarily performed by IRBs, contributes to patient safety by systematically reviewing studies for ethical compliance, ensuring that potential risks are minimized, and that participants are treated with respect and informed consent.
What measures are in place to protect the rights of participants in medical research?
To protect participant rights in medical research, measures such as informed consent, transparency about risks and benefits, and the right to withdraw from the study at any time are mandated to ensure ethical treatment and safety.
How do collaborative research initiatives like SMART IRB enhance patient safety?
Collaborative research initiatives like SMART IRB streamline the IRB review process, ensuring speedy and effective oversight across multiple sites. This enhances patient safety by facilitating compliance with ethical standards and reducing delays that could jeopardize research participant welfare.
What historical events have shaped the current framework of medical research safety?
Historical events, such as the Tuskegee Syphilis Study and unethical experiments during World War II, have led to the establishment of strict regulations and oversight mechanisms like IRBs to safeguard patient safety and uphold ethical standards in medical research.
How do IRBs help mitigate the risks of harm to clinical trial participants?
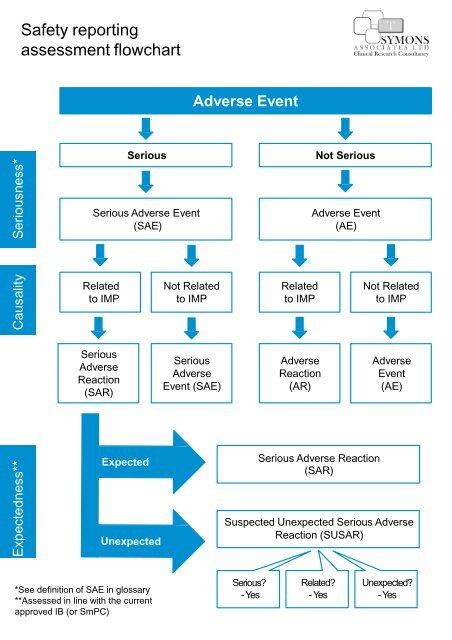
IRBs help mitigate risks by thoroughly evaluating research designs, ensuring informed consent processes are in place, and continuously monitoring studies for adverse events, ultimately safeguarding the health of clinical trial participants.
What challenges are faced in maintaining patient safety in medical research amid funding cuts?
Maintaining patient safety in medical research amid funding cuts presents challenges such as reduced oversight capabilities, delayed studies, and a potential increase in participant risks due to insufficient monitoring and loss of trust in the research community.
| Key Points | Details |
|---|---|
| Funding Cuts Impact | The Trump administration’s freeze of over $2 billion in federal research grants disrupts ongoing research and jeopardizes patient safety. |
| SMART IRB System | SMART IRB facilitates oversight of multi-site medical research, ensuring compliance and protections for research participants. |
| Role of IRBs | Institutional Review Boards (IRBs) review research proposals, assessments of risks, benefits, and ensure informed consent is obtained. |
| Historical Context | Past unethical research has led to the establishment of rigorous ethical standards and oversight in current medical research practices. |
| Impact of Delays | Halting studies midstream can cause harm to participants and erode public trust in medical research. |
| Current Efforts | Despite funding cuts, Harvard Medical School supports ongoing collaborative research essential for participant safety. |
Summary
Medical research safety is critical to protecting patients involved in studies. Funding cuts, like those imposed by the Trump administration, threaten these vital oversight systems, jeopardizing patient welfare and diminishing trust in research activities. Robust IRBs and funding mechanisms ensure ethical standards are upheld, safeguarding participants from potential risks. Continued investment in medical research not only protects individuals but also fosters progress in developing innovative treatments.