Maternal mortality rates in the United States remain a critical public health concern, particularly as they have persisted at alarmingly high levels compared to other high-income nations. Recent studies indicate that an overwhelming 80% of these pregnancy-related deaths are preventable, underscoring the urgent need for enhanced prenatal care and comprehensive postpartum support. Disparities in pregnancy care across various demographics, including race and geography, have led to significant differences in outcomes, especially among high-risk pregnancies. The need for improvements in maternal health is further amplified by the challenges posed by systemic racism, inadequate healthcare infrastructure, and insufficient access to pregnancy care services. As America grapples with these alarming statistics, it becomes increasingly clear that concerted efforts are necessary to eliminate preventable pregnancy deaths and foster equitable maternal health outcomes across all communities.
The topic of maternal mortality encompasses the vital issue of pregnancy-related deaths, shedding light on the overarching challenges within maternal health systems. In the U.S., elevated rates of death during and after childbirth signify a pressing need for reform in pregnancy care, particularly in addressing the stark disparities that exist among different racial and ethnic groups. The recent uptick in mortality highlights the critical need for comprehensive support throughout the postpartum phase, as many deaths occur beyond the traditional maternal mortality definition. As various studies reveal, high-risk pregnancies face unique barriers that shamefully contribute to fatal outcomes, necessitating a closer examination of America’s healthcare policies. Thus, improving maternal health is not just a medical imperative but a moral obligation that demands immediate action.
Understanding the Rise in Maternal Mortality Rates in the U.S.
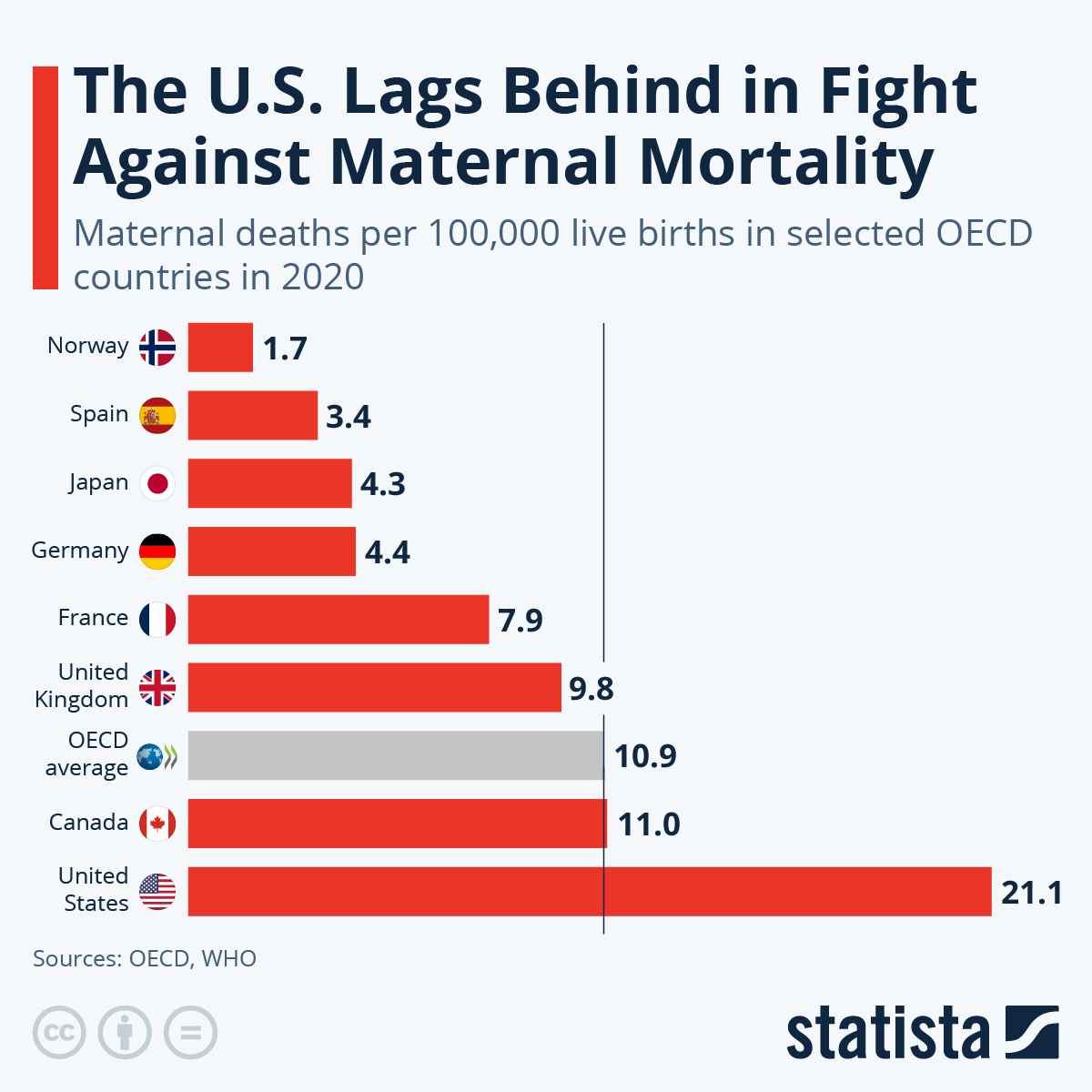
The United States continues to grapple with alarmingly high maternal mortality rates, particularly in comparison to other high-income nations. Despite advancements in medical technology and prenatal care, the U.S. faces substantial challenges in reducing preventable pregnancy deaths. According to recent studies, a staggering 80% of pregnancy-related deaths are avoidable, yet systemic issues within the healthcare system contribute to persistent vulnerabilities. The rising maternal mortality rate highlights the urgent need for comprehensive policy changes and a more equitable approach to maternal health.
Researchers have noted significant disparities in maternal mortality rates across different racial and ethnic groups, with American Indian and Alaska Native women experiencing mortality rates nearly four times higher than those of white women. These disparities are attributed to a combination of socio-economic factors, healthcare access, and chronic health conditions that disproportionately affect minority populations. Addressing these inequities is crucial for reducing maternal mortality rates and ensuring that all women receive the same standard of care.
The Role of Chronic Health Conditions in High-Risk Pregnancies
Chronic health conditions pose a significant risk factor for high-risk pregnancies, which can lead to increased maternal mortality rates. Conditions such as chronic hypertension and cardiovascular disease have been on the rise among younger populations, complicating pregnancy outcomes. Recent data reveals that women aged 25 to 39 exhibit a surprising increase in pregnancy-related deaths, indicating a troubling trend in the health of pregnant individuals. This underscores the need for targeted interventions to manage chronic health conditions prior to and during pregnancy.
In addressing high-risk pregnancies, healthcare systems must adopt a proactive approach that includes thorough screening and ongoing management of chronic diseases. Improved prenatal care strategies, accompanied by education on the importance of healthy lifestyle choices, can significantly impact outcomes. By focusing on early detection and management of risk factors, maternal health providers can help mitigate the risks associated with chronic conditions and ultimately reduce maternal mortality rates in the U.S.
Improving Postpartum Care to Reduce Maternal Deaths
The postpartum period is crucial for women’s health and well-being, yet it is often overlooked in maternal care discussions. Recent findings suggest that nearly one-third of pregnancy-related deaths occur during the late maternal period, which extends up to a year following childbirth. This highlights the importance of enhancing postpartum care and addressing the continuum of care that extends beyond the initial weeks after delivery. Failure to provide adequate postpartum care can lead to deteriorating health, particularly for those at high risk due to underlying chronic conditions.
Investing in comprehensive postpartum care, including mental health support and chronic disease management, can help reduce health complications for new mothers. Healthcare providers must ensure that women receive continuous support, ongoing assessments, and educational resources during the postpartum phase. By prioritizing postpartum care improvements, we can significantly decrease maternal mortality rates, ensuring that mothers have the necessary resources to thrive during this critical time.
Addressing Health Disparities in Maternal Care Systems
Health disparities have long plagued the maternal care system in the U.S., leaving marginalized groups at a disproportionately higher risk for negative pregnancy outcomes. Many women of color face barriers to accessing quality prenatal and postpartum care due to socioeconomic status, geographical location, and systemic biases within healthcare. These disparities exacerbate the already critical issue of maternal mortality, making it essential to implement equitable policies that address the root causes of these inequities and improve access to care.
To close the gaps in maternal health disparities, stakeholders must actively engage in community-based programs and policy reforms aimed at improving healthcare access for vulnerable populations. This includes addressing transportation barriers, expanding telehealth services, and fostering partnerships with community organizations to reach underserved communities. By focusing on equity in maternal health, we can reduce preventable pregnancy deaths and create a more inclusive healthcare environment.
The Impact of COVID-19 on Maternal Health Trends
The COVID-19 pandemic has significantly impacted maternal health trends, contributing to the rise in maternal mortality rates observed in recent years. Initial lockdown measures and strain on healthcare systems created new challenges for pregnant individuals, including limited access to prenatal care and heightened stress levels. These factors not only increase the risk of complications during pregnancy but also exacerbate existing health disparities within the community.
As we navigate the aftermath of the pandemic, it is crucial to address the lingering effects on maternal health. This includes reevaluating healthcare delivery systems to ensure that they are resilient and responsive to future public health emergencies. Implementing lessons learned during the pandemic—such as the integration of telehealth services—can enhance access to necessary care and provide ongoing support for expecting and new mothers, ultimately reducing mortality risks associated with high-risk pregnancies.
Innovative Solutions for Reducing Pregnancy-Related Deaths
To combat the rising rates of maternal mortality, innovative solutions in healthcare delivery are paramount. This includes the development of community-based programs tailored to support expectant mothers throughout their pregnancy journeys. Initiatives focusing on prenatal education, risk assessment, and individualized care plans can enhance outcomes and reduce preventable pregnancy deaths.
Collaboration among healthcare professionals, community organizations, and policymakers is essential to developing effective solutions that address the multifaceted challenges of maternal health. By leveraging real-time data to identify at-risk populations and implementing targeted interventions, we can create more robust healthcare frameworks that prioritize maternal well-being and significantly lower mortality rates across the nation.
The Importance of Tracking Maternal Deaths for Policy Improvement
Accurate tracking of maternal deaths is vital for understanding the root causes of maternal mortality and developing effective interventions. The implementation of standardized death certificates that include a pregnancy checkbox was a significant step in addressing the multi-faceted nature of maternal health outcomes in the U.S. This comprehensive data is essential for shaping policies that directly impact maternal care across different states and communities.
Despite improvements in data collection, there remains a need for continuous investment in maternal health research. Policymakers must prioritize funding for maternal health studies to inform evidence-based approaches to reduce mortality rates. By shining a light on the specific factors contributing to preventable pregnancy deaths, targeted initiatives can be deployed to tackle these issues and save lives.
Promoting Full-Spectrum Pregnancy Care to Save Lives
Full-spectrum pregnancy care encompasses a holistic approach to maternal health, addressing the needs of individuals from preconception through the postpartum period. This comprehensive care model recognizes the importance of continuity in healthcare, emphasizing the need for consistent support throughout pregnancy and after childbirth. By prioritizing full-spectrum care, health systems can better address the factors leading to preventable pregnancy deaths.
Integrating full-spectrum care within existing healthcare frameworks involves training providers in culturally competent practices and ensuring accessibility for all women. This means addressing logistic barriers and providing resources for families during the prenatal and postpartum phases. As we strive to enhance maternal health outcomes, promoting a full-spectrum approach is essential for reducing maternal mortality rates and improving the overall quality of care.
Advocacy for Maternal Health in Policy Making
Advocacy for maternal health is crucial in shaping policies designed to combat rising maternal mortality rates. Engaging stakeholders—including healthcare professionals, lawmakers, and community leaders—is essential to create meaningful change in the healthcare landscape. This advocacy must focus on elevating maternal health as a priority in local and national agendas, particularly for marginalized communities disproportionately affected by health disparities.
Effective advocacy involves raising awareness around the key issues contributing to maternal mortality, such as access to quality care, socio-economic barriers, and systemic biases in health systems. By fostering a collaborative approach and leveraging community voices, advocates can influence policy changes that promote equity and improve maternal health outcomes across varied demographics. Mobilizing support for maternal health initiatives is vital to ensuring the protection of new mothers and their babies.
Frequently Asked Questions
What are the primary factors contributing to high maternal mortality rates in America?
America’s maternal mortality rates are among the highest in high-income countries, largely due to a combination of inequitable healthcare access, systemic biases, inadequate prenatal care, and high rates of preventable pregnancy deaths. Chronic health issues, particularly cardiovascular disease, are increasingly affecting pregnant individuals, especially younger women, which further exacerbates these rates.
How do pregnancy care disparities impact maternal mortality rates?
Pregnancy care disparities significantly impact maternal mortality rates by creating unequal access to quality healthcare services. Women in states with fewer resources, maternity care deserts, and systemic discrimination face higher risks of preventable pregnancy deaths. Addressing these disparities is essential for improving overall maternal health and reducing mortality rates in high-risk pregnancies.
What improvements are suggested for postpartum care to reduce maternal mortality rates?
To reduce maternal mortality rates, particularly the increase in late maternal deaths, there is a need for improved postpartum care systems. This includes extending healthcare access beyond the traditional six-week postpartum period to ensure continuous monitoring and support for mothers during the critical year following delivery.
What role does addressing chronic health issues play in lowering maternal mortality rates?
Addressing chronic health issues, such as hypertension and cardiovascular disease, is crucial for lowering maternal mortality rates. With these conditions increasingly affecting younger individuals, targeted interventions before and during pregnancy are necessary to mitigate risks associated with high-risk pregnancies and improve overall maternal health outcomes.
How do state-level variations affect maternal mortality rates in the U.S.?
State-level variations significantly affect maternal mortality rates due to differences in healthcare access, policies, and quality of care. Some states, like California, demonstrate effective strategies in reducing pregnancy-related deaths, indicating that targeted state-level interventions can lead to substantial improvements in maternal health.
Why is it important to recognize late maternal deaths in discussions about maternal mortality rates?
Recognizing late maternal deaths—deaths occurring between 42 days and one year postpartum—is critical because they account for nearly a third of maternal deaths in the U.S. Considering this time period emphasizes the need for comprehensive care that addresses maternal health beyond the immediate postpartum phase, ensuring continued support for up to a full year after birth.
What are the implications of preventable pregnancy deaths on public health policy?
Preventable pregnancy deaths highlight significant gaps in public health policy, underscoring the urgent need for investment in maternal health infrastructure and targeted interventions. Policymakers must prioritize maternal health to develop effective strategies that reduce preventable deaths and ensure equitable access to quality pregnancy care across all demographics.
How has the COVID-19 pandemic influenced maternal mortality rates in the U.S.?
The COVID-19 pandemic has negatively influenced maternal mortality rates in the U.S., with a notable spike in 2021 linked to increased health complications and reduced access to care. This rise signifies the pandemic’s detrimental impact on pregnancy care and the importance of addressing such crises to improve maternal health outcomes.
What key measures can be taken to improve maternal health in the U.S.?
Key measures to improve maternal health in the U.S. include increasing investments in innovative healthcare solutions, enhancing access to high-quality prenatal and postpartum care, and addressing inequities in healthcare access. Comprehensive data tracking and policy reforms tailored to state needs are also vital to effectively reducing maternal mortality rates.
| Key Points | |
|---|---|
| High Maternal Mortality Rates in the U.S. | The U.S. has the highest maternal mortality rate among high-income countries, which continues to rise with significant differences among states, races, and ethnicities. |
| Preventable Deaths | More than 80% of pregnancy-related deaths are preventable. Changes in healthcare delivery and policy improvements are essential. |
| Key Findings of the Study | From 2018 to 2022, the rate increased from 25.3 to 32.6 deaths per 100,000 live births. Disparities were significant, especially among racial groups. |
| Leading Causes of Death | Cardiovascular disease accounted for over 20% of deaths, highlighting a shift in causes and the growing prevalence of chronic conditions among younger individuals. |
| Importance of Late Maternal Deaths | Late maternal deaths (deaths occurring between 42 days and one year postpartum) accounted for nearly one-third of total maternal deaths, indicating a need for better postpartum care. |
| Healthcare System Challenges | The U.S. healthcare system is plagued by inequities and insufficient infrastructures, leading to disparities in maternal health outcomes. |
| Call to Action | There is an urgent need to invest in public health infrastructure and innovative solutions to improve maternity care during pregnancy and postpartum periods. |
Summary
Maternal mortality rates in the U.S. have become a significant public health concern, particularly as they continue to rise within a landscape where over 80% of these deaths are deemed preventable. The latest data highlights alarming disparities not only among different ethnicities but also across states, suggesting systemic issues within the healthcare system that require urgent attention and reform. To mitigate these rising rates, it’s essential to enhance prenatal and postpartum care, address inequities in healthcare policy, and invest in research and public health initiatives that prioritize maternal health.